Impedance Tomography uses electrical signals to create images of organs. The images are reconstructed using relative and absolute impedance measurements. This article covers the basics of the technique. It also addresses the effects of PEEP on thoracic impedance. It also discusses the potential pitfalls of this technique.
Reconstruction from relative impedance measurements
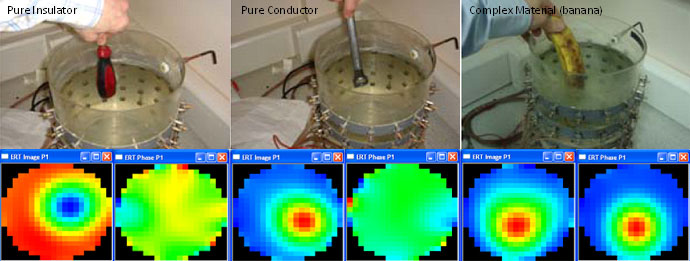
Reconstruction from relative impedance measurements is a method used to create an image of a patient’s impedance. The technique involves recording voltages on the surface of the thorax, and transforming this data into a representation of the patient’s impedance. The most common reconstruction algorithm is called the Sheffield back-projection algorithm. This algorithm has been modified a number of times.
Reconstruction from relative impedance measurements in electrical impedance tomography is a complex problem. The technique relies on a model that assumes the electrical current is a difference between two Neumann-to-Dirichlet boundary maps. However, the data cannot be perfectly modeled through numerical methods.
Effects of PEEP on thoracic impedance
In studies conducted on healthy patients, the effects of PEEP on thoracic imperfusion were not significant. However, in diseased patients, the PEEP-induced change in the total intrathoracic volume (ITP) must be considered. The amount of edema within the diseased lung may result in an increase in the ITP while the amount of aerated lung may decrease. These changes in ITP determine the hemodynamic effects of PEEP.
Increasing the PEEP in patients with acute lung injury could increase the ITP, even if it has minimal effects. In addition, the Pes may provide a reliable estimation of changes in Ppl and Ppc, but these measurements may underestimate these changes when lung volumes increase. Thus, the most important question is how the PEEP affects ITP and total lung volume.
Effects of PEEP on thoracic impedance measurements
PEEP is a common therapeutic method for patients suffering from a heart attack. It is used to elevate preload and improve myocardial contractility. It is important to understand that this treatment can affect coronary perfusion. Nevertheless, it is not clear whether PEEP is harmful to the heart. In fact, studies have shown that PEEP levels up to 15 cm H2O do not seem to reduce myocardial contractility and work. This suggests that the direct effects of mechanical ventilation are not nearly as important as their effects on pre and afterload.
The LIVE trial showed that patients with focal ARDS responded better to low PEEP compared to diffuse ARDS patients. Higher PEEP was associated with lower COVID-19 levels in diffuse ARDS patients. This research demonstrates that adjusting PEEP can help improve the patient’s lung function.